Juli Engel was delighted when a neurologist recommended a PET scan to determine whether amyloid — the protein clumps associated with an increased risk of Alzheimer’s disease — was accumulating in her mother’s brain.
“My internal response was, ‘Yay!’” said Ms. Engel, 65, a geriatric care manager in Austin, Tex., who has been making almost monthly trips to help her mother in Florida. “He’s using every tool to try to determine what’s going on.”
Sue Engel, who’s 83 and lives in a retirement community in Leesburg, Fla., has been experiencing memory problems and other signs of cognitive decline for several years. Her daughter checked off the warning signs: her mother has been financially exploited, suffered an insurance scam, caused an auto accident.
Medicare officials decided in 2013, shortly after PET (positron emission tomography) amyloid imaging became available, that they lacked evidence of its health benefits. So outside of research trials, Medicare doesn’t cover the scans’ substantial costs ($5,000 to $7,000, the Alzheimer’s Association says); private insurers don’t, either.
Juli Engel thinks Medicare should reimburse for the scan, but “if necessary, we’ll pay for it out of pocket,” she said.
Her mother already has an Alzheimer’s diagnosis and is taking a commonly prescribed dementia drug. So she probably doesn’t meet the criteria developed by the Alzheimer’s Association and nuclear medicine experts, which call for PET scans only in cases of unexplained or unusual symptoms and unclear diagnoses.
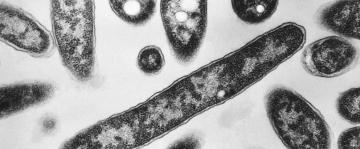
But as evidence mounts that brain damage from Alzheimer’s begins years before people develop symptoms, worried patients and their families are turning to PET scans to learn if they have this biomarker.
They have few alternatives. Scientists at Washington University in St. Louis announced on Thursday that they’ve developed a blood test for amyloid that can predict the development of plaques in the brain, but it is years away from use in doctors’ offices.
Some experts fear PET scans offer few benefits, at substantial costs. “There are lots of incentives, including financial incentives, for doing more testing and interventions,” said Dr. Kenneth Langa, a researcher at the University of Michigan and author of a recent article in JAMA Internal Medicine about diagnosis of early Alzheimer’s disease. “My hope is we’ll think hard about the unintended downsides.”
What downsides? Amyloid plaques occur commonly in older people’s brains, but not everyone with amyloid will develop dementia, which probably involves multiple factors. Nor does a negative PET scan mean someone won’t develop dementia.
Biostaticians at the University of California, Los Angeles, have calculated that a 75-year-old man with amyloid has a 17.2 percent lifetime risk of developing Alzheimer’s dementia; for a woman that age, with a longer life expectancy, the figure is about 24 percent.
That’s primarily because Alzheimer’s rates climb steeply at older ages, when people grow more likely to die of other causes before they can develop symptoms. (With additional biomarkers, or with the condition called mild cognitive impairment, the lifetime risk rises.)
But older people may also be among the 30 percent or so of those with amyloid deposits who, for unexplained reasons, retain normal cognition.
“If we start treating everyone with preclinical Alzheimer’s, we’ll treat a lot of people who would never have gone on to have dementia at all,” Dr. Langa said.
Moreover, what treatments would those be? Multiple trials have failed to find drugs that prevent, reverse or slow Alzheimer’s disease, perhaps because these treatments were introduced too late in the disease’s course.
Results from a different approach, an infusion drug being tested in older people with amyloid but without cognitive impairment, remain several years away.
“As a clinician, would I like amyloid information about my symptomatic patients? Yes,” said Dr. Ronald Petersen, a neurologist and director of the Mayo Clinic Alzheimer’s Disease Research Center. “Am I going to be able to do something about it? Not at present.”
The drugs approved for Alzheimer’s, primarily Aricept and Namenda, have modest benefits in some patients for a limited time. Neither has been shown effective for mild cognitive impairment, often a precursor to dementia.
Yet a recently published study, undertaken to provide Medicare with more information in hopes of reversing its reimbursement decision, shows that positive amyloid PET scans lead to far greater use of these and other medications.
The Ideas study (the name is shorthand for “Imaging Dementia — Evidence for Amyloid Scanning”) analyzed the treatment of 11,409 Medicare beneficiaries with mild cognitive impairment or dementia (average age: 75) nationwide. PET scans detected amyloid in 55 percent of the patients with mild impairment and 70 percent of those with dementia; those results influenced their cases in several ways.
The biggest change: soaring prescriptions. About 40 percent of those with mild impairment had been taking Alzheimer’s drugs; after a PET scan that detected amyloid plaques, the proportion more than doubled. In those with dementia, use of dementia drugs climbed from 63 to 91 percent after a positive PET scan.
Stopping those drugs after a negative scan happened far more rarely, “a very common dynamic in medicine,” Dr. Langa pointed out. “Once a treatment is started, it’s hard to stop it.”
The second round of the Ideas study will assess whether these changes led to better health. Were patients less likely to go to emergency rooms or to be hospitalized? Did costs rise or fall?
The researchers expect to publish those findings early next year. If they show that patients benefited, the Alzheimer’s Association will ask Medicare to reconsider its earlier decision and cover PET scans for the subset of patients with atypical or unexplained symptoms.
Those questioning broader access worry, however, about “indication creep,” when a drug or test approved for patients with a particular condition becomes used for others. They also worry about crushing costs for Medicare.
“Even if a scan cost zero dollars, I wouldn’t recommend it,” said Dr. Ken Covinsky, a geriatrician at the University of California, San Francisco. “Do you really want to know that you have amyloid in your brain, years ahead of cognitive problems that may never develop?”
Proponents of making PET scans more widely available argue that knowing their amyloid status may motivate patients to make lifestyle changes. Stopping smoking, exercising and eating more healthily are all found to reduce dementia, even among those at higher genetic risk. Perhaps, too, patients will be more likely to begin advance care planning.
“Those are good things to do whether you have amyloid or not,” Dr. Covinsky argued.
For now, costs probably prevent many people from seeking PET scans for diagnosis. If Medicare will pay — and possibly even if it won’t — more patients may find ways to be scanned.
“You’ll always have people who use it inappropriately, but hopefully we can keep that to a minimum” by educating doctors, said Maria Carrillo, chief science officer at the Alzheimer’s Association.
But ultimately, “we’re not here to tell people what to do,” she added. “There are people who really want that validation, and that’s a personal decision.”
Juli Engel may be among them.
Once the neurologist documents her mother’s incapacity, she can take steps to prevent Sue Engel from driving, and to move her into assisted living when needed. As a geriatric care manager, “I know the trajectory of this disease,” she said.
Because she also knows that both her maternal grandparents had Alzheimer’s, she is considering her own future, too. Does she have amyloid in her brain?
Her family is full of scientists, and “it’s our bent to want to know these things,” she said. “I think we’re entitled to that.”