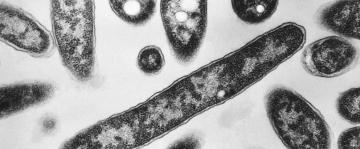
MADRID -- Zoilo Patiño was just one of more than 19,000 elderly people to die of coronavirus in Spain’s nursing homes but he has come to symbolize a system of caring for the country’s most vulnerable that critics say is desperately broken.
When the Alzheimer’s-stricken 84-year-old succumbed in March on the same day 200 others died across Madrid, funeral homes were too overwhelmed to take his body and he was instead left locked in the same room, in the same bed, where he died.
Spanish army disinfecting teams going through the Usera Center for the Elderly more than 24 hours later were stunned to come across Patiño’s body and it made headlines around the world, with the country’s Defense Minister Margarita Robles describing “elderly abandoned, if not dead, on their beds.”
“It wasn’t ideal to have a possibly infectious body there,” says José Manuel Martín, a staff member who took the soldiers through the home. “But what else could we have done? We didn’t even have protective gear to be able to put the body in a bag.”
The grim find triggered soul-searching over Spain’s nursing homes, which have had more deaths than those in any other country in Europe. Much of the scrutiny has focused on the lower end of the market, government-owned homes like the Usera center, where day-to-day operations have been contracted to companies often controlled by multinational private-equity firms that seek to turn profits quickly by cutting staff, expenses —and some say care — to the bone.
An Associated Press investigation into the 160-bed nursing home where Patiño and 41 others died revealed widespread cost-cutting for years leading up to the pandemic and a series of questionable decisions at the height of the crisis. That included the facility’s top doctor admonishing workers for weeks not to wear masks, and allowing six crucial days to pass before complying with a government order to separate the sick from the well.
Dozens of interviews with workers, relatives and residents themselves, along with publicly available documents, painted a picture of a stripped-down, “fast-food” version of elder care. They described broken equipment, missed medications and nurse’s assistants responsible for caring for 10 or more residents at a time, with meals often cut short and some residents told to wear diapers to reduce trips to the bathroom.
The private company that operates Usera disputed AP’s reporting of poor care and declined to comment on calls by elder care watchdogs and others to reform a system that puts private-equity profit incentives on public nursing homes.
“This model is not working.” Alberto Reyero, the top Madrid regional government official in charge of elder care, warned in February, barely a month before the new virus spread like wildfire through the capital’s nursing homes.
“We have to find another way.”
———
A cacophony of coughing echoed through the Usera center on the morning of March 12, with dozens of residents falling ill to fevers and other flu-like symptoms.
But an existing protocol in the home to deal with infectious outbreaks had yet to be implemented. Masks, gloves and other protective gear weren’t mandated, and testing for COVID-19 was something employees had only seen on TV.
That morning, wearing a mask she bought herself, an auxiliary nurse set out for the top floor of the four-story, red-brick center where the sickest residents were staying. Halfway up the stairs, she ran into the facility’s doctor.
“’Take off that crap, it’s useless,’” the nurse, who asked that her name not be used for fear of reprisal, says she was ordered. “He said all I was doing was scaring the residents.”
On March 16, after Patiño woke up with a fever, difficulty breathing and no appetite, the Usera center’s physician convened a meeting to inform workers that a first suspected coronavirus case had been detected on the premises. Those in attendance say they were reminded again that the policy was still to avoid using masks, with the doctor playing a recording of somebody he presented as an expert saying they were useless and would only spread panic.
Four days later, Patiño became one of the first residents to die at Usera, and then the deaths began coming in twos and threes a day.
On March 21, the Spanish government ordered an immediate separation of nursing home residents into four groups: those infected, which was something nearly impossible to confirm given that no testing kits were available; those with symptoms; those suspected of having had contact with a positive case; and those who appeared healthy.
The order was meant to be carried out in 24 hours. But by then at least 30 workers were ill, and according to internal documents reviewed by AP, the separation didn’t begin until March 27, six days after the order was issued.
By the end of March, 18 people had died. And twice as many would die in the following days.
The auxiliary nurse who had first been told to scrap her mask described the situation inside the facility as “unsustainable.”
She also began feeling dizzy with difficulty breathing before she tested positive for the virus herself, among about half of the Usera center’s staff of 131 who would eventually fall ill to COVID-19.
“When they should have been protecting all of us workers and residents, they basically left us exposed, abandoned.”
———
Nursing homes have become a flashpoint in the global pandemic, with more than a third of the U.S.’s 100,00 deaths in such facilities, and higher proportions reported in such countries as Canada, Ireland and France. Spain’s more than 19,000 nursing home deaths is out of an official overall death toll of about 27,000, but that is likely an undercount because it includes only those who tested positive. Some estimates put the actual toll as high as 43,000.
Spain’s 4.5 billion-euro ($4.9 billion) eldercare industry has 373,000 elderly people in more than 5,400 nursing homes, and it has increasingly become profit-driven, with 7 out of 10 beds privately run.
Nearly 45% of the remaining public ones, around 45,000 beds, are additionally offered to be managed by private companies, the vast majority of which are backed by domestic and foreign private-equity firms eager to get a return on typically short-term investments.
Whether these public homes, like the Usera center, were hit harder than privately owned ones in the coronavirus pandemic is not clear, since the Spanish government has yet to break down death and infection numbers by specific homes. But some of the biggest outbreaks that have been publicized are in homes that are government-owned and privately operated. In the Madrid area alone, another facility managed by the same company as Usera saw at least 46 deaths, and two nursing homes managed by a competitor recorded 96 and 27 deaths, respectively.
Joseba Zalakain, director of SIIS, a research center focused on social issues, says that Spain’s public nursing homes managed by these multinationals are, as a rule, “centers with few resources that are very badly equipped, squeezing the idea of the low-cost so much that they are crippled to react to something like a pandemic.”
But private operators point fingers at the underfunding of nursing homes by the government, and the fact that coordination with the national health system is poor. José Ramón Repullo, an economist at Spain's top health institute, Carlos III, says the blame is shared. “If the state is awful at managing these facilities, it’s even worse at supervising them,” he says.
At the Usera center, a publicly-owned facility in a working-class section of Madrid, the first changes came in 2012 after Quavitae, a growing player in Spanish elder care backed by a British private-equity fund, won the contract to operate the home with the lowest bid. It came in 2 million euros ($2.2 million) below the 11.5 million euros ($12.6 million) that officials calculated that running the facility for four years would cost.
María Mendoza, who has worked at Usera for 12 years as an auxiliary nurse, said the new owners imposed staff cuts almost immediately and “everything went downhill from there.”
They decided a doctor during the night shift was no longer needed, and that they could get by with fewer nurses. Mendoza says the facility’s maintenance also was kept to a minimum. A toilet or an elevator would break and go unrepaired for weeks. There were leaks. And cranes used to lift residents from their beds would break and not be fixed.
“The place started to fall apart,” Mendoza says.
By the end of 2016, Usera’s management changed hands when Quavitae sold its nursing home operations to DomusVi, which was founded by one of France’s richest businessmen, Yves Journel. It has since become Spain’s leading private operator of nursing homes, with more than 20,000 beds in over 150 facilities.
DomusVi’s majority stake was held at the time by the French private equity firm, PAI Partners, which sold out just months later to the London-based private-equity firm, ICG. Soon after, ICG applied to refinance 1 billion euros in debt.
All that churn meant further cuts at Usera at a time when studies showed that the elderly moving into such facilities were increasingly dependent on additional help. Auxiliary nurses who do most of the hands-on patient work were the biggest cutback since the private equity-backed firms took control at Usera, dropping from 43 to 32 overall, with no more than 17 on at any one shift.
“The ratio became pretty much one auxiliary nurse for every 10 elders,” says Florencia Yacovano, who has been a receptionist at the Usera center for more than a decade. “Imagine rushing to get 10 of them out of bed, showering them and dressing them in just over one hour, in time for breakfast. It’s literally impossible.”
Beatriz Cano, a 70-year-old who has lived in the home for more than a decade with a chronic illness, says staffing constraints caused residents to be showered every other day rather than daily; they were told to limit toilet use and wear diapers in off hours; and there was little patience for those needing extra help to eat.
“If someone needs half an hour to be fed slowly … it’s just easier to give up after two spoonfuls and write down that the resident has no appetite today,” she says.
Esther Navarro says her 97-year-old mother was given sleeping pills in the morning, rather than at night, without justification, and staff would leave the woman in bed, sometimes until the afternoon. More than once she found her mother’s pills on the floor.
“The feeling of my siblings and myself, when leaving the residence, was always the same — they are cheating us, they are laughing at us.” Navarro added. “We always felt frustration and helplessness.”
The complaints finally caught the regional government’s attention. DomusVi was fined 83,400 euros ($91,800) last year for not meeting the technical requirements of its contract and specifically for the lack of maintenance of the facilities. Years earlier, they had been fined for having insufficient personnel and for failing to make agreed-upon improvements.
AP learned that on Feb. 26, three DomusVi executives were called to the regional government offices and informed that their contract would be taken away for their latest offense, outsourcing the employment of nurses. They were told it would be a matter of paperwork over a few weeks before it was settled.
Then the coronavirus struck.
Mendoza, the auxiliary nurse, says there seemed to be a shift after it became clear DomusVi was about to be permanently replaced.
“Because this company already had one foot outside," she says, "they didn’t give a damn about us."
———
In an email, DomusVi rejected all claims made to AP by workers, relatives and residents at the Usera nursing home, saying it took measures to face the coronavirus “since the end of February,” handled Patiño’s body properly and separated residents according to their symptoms “in the stipulated time.”
DomusVi refused to comment on the government’s decision to strip its Usera contract and the broader criticism of public-private partnerships. It said nursing homes have been “unfairly” criticized during the pandemic when many coronavirus deaths happened in hospitals, adding “it is the health system that has to cure residents.”
ICG — the private-equity firm that has lent to or invested in hundreds of companies, including a British software firm, an Italian drug maker and a French supplier of fasteners — defended DomusVi as a “high-quality business.” ICG added it is “doing everything we can to support the businesses that we invest in."
Last month, over 1,000 academics and civil society leaders signed a manifesto calling for an “urgent revision” of the long-term care model and its “corresponding scenario of public funding.”
Responding to part of the criticism, the Madrid government told the AP that the pandemic “has shown that a new model is necessary” that guarantees appropriate health care in nursing homes. "A model that focuses on the needs of the people, who now have a longer life expectancy and live their last years with a higher level of dependency.”
This month, dozens of relatives of those who died in 15 Madrid nursing homes, sued the regional government and individual home directors, accusing them of reckless homicide, degrading treatment, abuse of power and denial of help.
Several plaintiffs were families who had loved-ones in Usera, including Elena Valero, whose father died of COVID-19 and whose mother recovered from it.
If any good can come out of the crisis, she says, it would be an overhaul of the elder care system in Spain.
“What we want is that the model goes from being hostels where they are fed and given a bed, run on the cheap, to residences with proper health and social care, with dignity.”
———
AP investigative reporter Bernard Condon in New York contributed to this report.
———
Follow AP pandemic coverage at http://apnews.com/VirusOutbreak and https://apnews.com/UnderstandingtheOutbreak