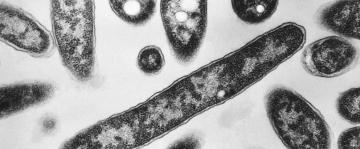
Less than two years ago, county officials in Los Angeles warned that deadly disease outbreaks were becoming a “serious threat” and that the county’s public health system still suffered from “gaps” in “strategy” and “resource preparation,” including a “limited number of ventilators.”
“Los Angeles County is one of the most vulnerable to an emerging infectious disease threat,” the local authorities wrote in a July 2018 report.
Indeed, as the COVID-19 crisis continues to unfold, Los Angeles County has become one of the hardest-hit counties in the nation, enduring more than 1,000 deaths and more than 20,500 cases so far.
The 2018 report is one of dozens of documents reviewed by ABC News that show governors and local authorities were keenly aware even years ago that when a pandemic inevitably hit, they would endure life-threatening shortages and receive limited help from the federal government.
“[States] are not yet adequately prepared,” declared a 2008 report by the National Governors Association (NGA), which noted that a pandemic could “overwhelm” U.S. hospitals, “severely impact” state economies, threaten food supplies, and shutter schools and universities.
But the documents reviewed by ABC News and interviews with several current and former government officials expose a painful paradox about preparing for a pandemic: States could have been far more self-reliant, but only if the federal government had provided more help.
After all, states and local jurisdictions were never expected to prepare for a pandemic in the same way the federal government was supposed to be ready, according to the current and former officials.
“It’s important for states to have adequate inventory to get started, but this thing was so big that it quickly outstripped any reasonable state efforts,” said Janet Napolitano, the former Arizona governor who then served as President Barack Obama’s Homeland Security secretary. “Ensuring that the country as a whole has what it needs to get control of this thing is a federal duty.”
President Donald Trump watches as Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, speaks about the coronavirus in the James Brady Press Briefing Room of the White House in Washington, April, 22, 2020.
President Donald Trump watches as Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, speaks about the coronavirus in the James Brady Press Briefing Room of the White House in Washington, April, 22, 2020.Alex Brandon/APAnd, as described by Napolitano, states prepare for pandemics based on two key assumptions: that U.S. officials – backed by the U.S. intelligence community – will tell them when a deadly disease is actually on its way, and that U.S. officials will establish “a national testing plan” to track the disease once it reaches U.S. soil.
The fact that neither happened at the start of the coronavirus crisis amounts to a “basic failure” by the federal government, according to Napolitano. “Right now it’s just chaos out there.”
But the federal government doesn’t deserve total blame for what has unfolded, according to Daniel Kaniewski, who until January served as a deputy administer at the Federal Emergency Management Agency (FEMA).
By law, the federal government is just a back-up system to states, so “the reality is that all levels of government need to be prepared for something like this,” he said.
Earlier this month, President Donald Trump called his administration "the greatest backup that ever existed for the states," even as he acknowledged governors were struggling to find more ventilators, testing kits, and other critical supplies.
‘The scale of 9-11’
In 2006, two years before releasing a second report on the issue, the NGA’s Center for Best Practices published what its then-director now calls a “prescient” booklet.
“It was all covered, it was all there,” John Thomasian said of what’s unfolding 14 years later in the midst of the coronavirus crisis.
FDNY paramedic Elizabeth Bonilla drives to an emergency call along an empty street on her second consecutive shift on April 15, 2020, in the Bronx borough of New York City. "The moment we walk through the door, the families, it's almost like they've seen God," Bonilla said. "They are looking for help immediately. They have this sense of relief, and then they go ahead and pass all responsibility on you. You want to make sure you're strong for them."
FDNY paramedic Elizabeth Bonilla drives to an emergency call along an empty street on her second consecutive shift on April 15, 2020, in the Bronx borough of New York City. "The moment we walk through the door, the families, it's almost like they've seen God," Bonilla said. "They are looking for help immediately. They have this sense of relief, and then they go ahead and pass all responsibility on you. You want to make sure you're strong for them."John Minchillo/APTitled “Preparing for a Pandemic Influenza: A Primer for Governors and Senior State Officials,” the 23-page booklet warned that, “When a pandemic occurs, the impact of the disease will join the lexicon of nation-changing incidents on the scale of 9-11.”
At the time, states – and the federal government – were still shaken by the SARS outbreak a few years earlier and concerned that the growing spread of Avian flu might turn into a pandemic.
“[T]he federal government does not stockpile doctors or nurses,” so “states will be expected to” coordinate care for patients when hospitals are filled, provide food to those who need it, and make “decisions on closings and other efforts to limit public gatherings,” the NGA cautioned.
“Under any realistic scenario, the federal government will have limited resources to devote to a pandemic,” the NGA added. “It is better to plan for self-reliance and utilization of state-based assets for state and local responses.”
One way to become more self-reliant: “Stockpile equipment and supplies which may be in short supply such as masks, ventilators [and] hand sanitizers,” the NGA said.
In this March 17, 2020, file photo, boxes of N95 protective masks for use by medical field personnel are seen in New York.
In this March 17, 2020, file photo, boxes of N95 protective masks for use by medical field personnel are seen in New York.Mike Segar/Reuters, FILEBolstered by federal grants, many states did what they could over the next few years, drawing up pandemic response plans for the first time, holding exercises to expose problems and build important relationships, and purchasing limited amounts of potentially live-saving supplies such as ventilators and vaccines.
California spent $200 million to stockpile 50 million masks, set aside 2,400 portable respirators, and even build three 200-bed "mobile hospitals," according to a recent Los Angeles Times report.
“It is absolutely a critical investment,” then-Gov. Arnold Schwarzenegger, R-California, said at a press conference in June 2006. “I’m not willing to gamble with the people’s safety.”
‘A new bottom line’
But despite the “robust response from most states” to growing concern about pandemics, some states “just made very deliberate decisions” not to stockpile critical supplies, Mike Leavitt, then the U.S. Health and Human Services Secretary, told Congress in February 2008.
He worried “that sometimes our effort at the federal level causes the state and local governments to not view this as a priority,” he said.
And the nation’s growing financial crisis at the time likely exacerbated that issue, according to current and former officials.
“Particularly after the ‘Great Recession,’ funding for public health departments has been constrained, and that’s led to a kind of fragile public health infrastructure at the state and local level,” Napolitano said.
Janet Napolitano, president of the University of California, speaks during a hearing, July 29, 2015 in Washington.
Janet Napolitano, president of the University of California, speaks during a hearing, July 29, 2015 in Washington.Astrid Riecken/Getty Images, FILEStates were “crushed” by the economic downturn, and – after reaching a peak after Hurricane Katrina in 2005 – federal grant money to support local preparedness efforts was cut by as much as 80 percent in some states, according to one state’s emergency management director.
Those reductions created “a new bottom line” for state budgets, which left health preparedness programs under-appreciated and underfunded, the official said, speaking to ABC News on the condition of anonymity so he could talk freely.
Tune into ABC at 1 p.m. ET and ABC News Live at 4 p.m. ET every weekday for special coverage of the novel coronavirus with the full ABC News team, including the latest news, context and analysis.
Indeed, in December 2008, South Carolina’s Department of Health issued a report saying: “Federal funding for the pandemic influenza preparedness program has ended, and no state funds have been appropriated to continue public health preparedness efforts for pandemic influenza.”
Less than three years later, California cut off the money to store and maintain its much-touted stockpile of ventilators and critical supplies, the Los Angeles Times reported.
‘An unspoken trend’
Craig Fugate, who headed FEMA under president Barack Obama’s administration, told ABC News that after taking over the agency in 2009 and in the years since, he “noticed an unspoken trend from states to let the federal government handle” key parts of pandemic preparedness.
Other former federal officials described witnessing a similar tendency.
“I’ve seen a lot of governors say, ‘Well, we’re just going to get it from the feds when we have a problem,’” recalled George Foresman, who was the nation’s first preparedness chief at the Department of Homeland Security when George W. Bush was president.
But that state-level mindset is often based on “an outsized perception of what the federal government [really] has” – the Strategic National Stockpile was built to handle a limited “series of regional events,” not “a full-scale, border-to-border crisis,” Foresman said.
A funeral worker is assisted moving a deceased patient into a van at the Brooklyn Hospital Center on April 27, 2020, in New York.
A funeral worker is assisted moving a deceased patient into a van at the Brooklyn Hospital Center on April 27, 2020, in New York.Stephanie Keith/Getty ImagesEven the state emergency management director who spoke on the condition of anonymity conceded "reliance on the Strategic National Stockpile was always the plan for all the states."
Meanwhile, Thomasian said many states grew “complacent” over time.
“Do I think they were prepared then better than they are now? Yes,” he said, noting that recurring changes in state leadership over many years meant “a lot of collective memory got lost on issues around the pandemic.”
Some states even stopped conducting drills as often, he added.
“The last several years have been all about hurricanes, wildfires, cybersecurity, domestic terrorism, active shooters,” the state emergency management director said. “Attention and preparedness followed.”
Nevertheless, state and local governments continued to recognize what the NGA first warned about in 2006: the federal government may be of little help when a pandemic inevitably struck.
“Medical materials like PPE, medications and ventilators may not be available from the Strategic National Stockpile,” said the report from Los Angeles County in July 2018.
The statewide plan for Illinois issued in 2014 stated: “Although planning has occurred … [there] might be shortages of items, such as gloves, respirators, ventilators and laboratory testing supplies.”
New York and several other states even established guidelines laying out how hospitals should allocate ventilators during a pandemic, “when there are insufficient ventilators to treat everyone who needs them,” as New York’s health department said in a press release in 2015.
‘A renewed interest’
In an ideal world, states would have infinite amounts of money to purchase enough ventilators and masks for each citizen when a pandemic hits.
In late March, as New York's Democratic governor, Andrew Cuomo, pleaded for help finding more ventilators, Trump said Cuomo "should have ordered the ventilators [years ago]. He had a choice."
Jim Malatras, President of SUNY Empire State College, left, listens as New York State Governor Andrew Cuomo, right, speaks during his daily coronavirus press briefing at SUNY Upstate Medical University, April 28, 2020 in Syracuse, New York. Cuomo detailed guidelines to reopening parts of New York State around May 15, 2020.
Jim Malatras, President of SUNY Empire State College, left, listens as New York State Governor Andrew Cuomo, right, speaks during his daily coronavirus press briefing at SUNY Upstate Medical University, April 28, 2020 in Syracuse, New York. Cuomo detailed guidelines to reopening parts of New York State around May 15, 2020.Stefani Reynolds/Getty ImagesBut governments will spend themselves "into oblivion by chasing the ideal" of the "perfect" amount of equipment, Foresman said.
So, facing other more likely natural disasters, governors “have to hedge their bets,” according to Kaniewski.
Factoring into their gamble: Governors have become “overly confident” that if a catastrophic event unfolds, the federal government will issue a “disaster declaration” and reimburse them for as much as 75 percent of their state’s response costs, one former FEMA official told ABC News, speaking on the condition of anonymity.
“But that’s the wrong way to look at it,” the former FEMA official insisted. “States need to be proactive in reducing the impact of disasters before they happen.”
According to Fugate: "States should do more, even if Congress must fund it."
Still, the true “measure of performance in a crisis is not whether you have resource shortages,” it’s “whether you have systems in place” to minimize the impact of those shortages, according to Foresman.
Under the coronavirus crisis, "there is no system in the world that would have [prevented shortages] when we’re competing on a global scale for PPE or ventilators," he said.
As Napolitano sees it, the latest pandemic will spur states to take more action.
“I suspect that one of the things that will emerge from the COVID-19 pandemic is a renewed interest in building up the public health infrastructure,” she said.
Foresman agreed.
“There’s a lot of tragedy in this pandemic," he said, "but one of the positive things that comes for societies in the aftermath of a crisis is that they are better prepared for the next event when it occurs.”
The NGA did not respond to multiple emails seeking comment for this article. An email to Cuomo's office was also not returned.