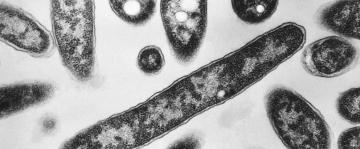
Photo: Stuart Monk (Shutterstock)
With COVID cases on the upswing again (we’re on, what, the fifth wave? The seventh?) it’s important to know that there’s a medication that can prevent severe disease in people who are at high risk of complications. It’s called Paxlovid. But not everyone is eligible to receive it. Here’s how to find out if you qualify.
What is Paxlovid?
Paxlovid is a brand name for a combination of two generic medications. One is nirmatrelvir, which blocks an enzyme that the COVID virus needs to replicate. The other is ritonavir, which blocks one of our own enzymes that would otherwise break down the nirmatrelvir. (Ritonavir is also used this way with antivirals that treat HIV.)
Paxlovid was granted an emergency-use authorization by the Food and Drug Administration in December 2021. That makes it relatively new, and if you haven’t heard of it, you’re not alone. Many people who could qualify for it don’t realize that they can ask for it, and not all doctors will recommend it.
When can you take Paxlovid?
The most important thing to know about getting Paxlovid is that it needs to be started within five days of when you first started experiencing symptoms. If a week passes before you consider seeking treatment, it’s too late for Paxlovid to help you.
The drug is also not authorized for people who are already hospitalized for severe COVID-19.
Who can take Paxlovid?
Paxlovid is approved for people who are at least 12 years old and weigh at least 88 pounds. Because there isn’t much of the stuff available, it’s currently only authorized for people who are at high risk of developing severe disease. This includes:
Everyone 65 and olderPeople with cancerPeople with certain chronic diseasesPeople with heart diseasePeople with diabetesPeople who are immunocompromisedPeople who are physically inactivePeople who are considered “overweight” or “obese”Current and former smokersThis isn’t a complete list; the CDC has a list here of conditions that make people more susceptible to severe COVID-19. This also doesn’t operate as a strict checklist. If your doctor decides you are high enough risk to benefit from a course of Paxlovid, then you qualify for the drug.
What are the risks associated with taking Paxlovid?
Because ritonavir interferes with an important liver enzyme, you should not take it if you are also taking a medication that depends on that enzyme or that inhibits that enzyme. Here is a list of drugs that are not compatible with Paxlovid. They include some medications for heart conditions, high blood pressure, and psychiatric medications, as well as St. John’s Wort. It’s important to discuss all your medications and supplements with the provider prescribing Paxlovid for you.
Paxlovid is usually “well-tolerated,” meaning it doesn’t cause serious health problems. But side effects can include diarrhea, increased blood pressure, muscle aches, and a temporary change in your sense of taste (usually causing a metallic taste).
There are also signs that Paxlovid may cause a “rebound,” in which viral levels increase after you’re done with the five-day course. This is still being studied. We don’t know yet how often this happens, nor whether it would help to take a longer course of the drug or to take it a second time.
How can you get Paxlovid?
Paxlovid is a prescription drug and you need to qualify for it, so you’ll need to talk to a provider. If you have a family doctor you can reach out to, that would be a good place to start.
Otherwise, use the Test-to-Treat locator to find pharmacies and clinics where you can get a COVID test (or show them your at-home test results) and get a prescription the same day. You can also call 1-800-232-0233 (TTY 1-888-720-7489), or call the Disability Information and Access Line at 1-888-677-1199 or DIAL@usaginganddisability.org. Check your local options as well: for example, New York City has a program that can deliver Paxlovid to your door if you qualify.