HARTFORD, Conn. -- The Abbott Terrace Health Center in Waterbury, where 41 residents have died from the coronavirus, has been cited by regulators for infection control violations and fined three times by the state and federal governments over the last several years. It has the lowest nursing home overall rating issued by the federal government — one star, for “much below average.”
About 40 miles (65 kilometers) away, the Kimberly Hall North nursing home in Windsor has the highest rating, five stars, issued by the Centers for Medicare & Medicaid Services. It has had one infection control citation, but no state or federal fines, over the past several years. Yet 43 residents there have died from the virus.
The coronavirus has had no regard for health care quality or ratings as it has swept through nursing homes around the world, killing efficiently even in highly rated care centers.
Preliminary research indicates the numbers of nursing home residents testing positive for the coronavirus and dying from COVID-19 are linked to location and population density — not care quality ratings — said Vincent Mor, professor of health services policy and practice at Brown University’s School of Public Health.
“It is not necessarily related to the good star, bad star ... of the home,” Mor said, “because really good homes, they have staff who go home and they are going to be living in an environment with lots of COVID and the staff will bring it in with them.”
In a study funded by the National Institute on Aging, Mor and fellow researchers reviewed data from nursing homes in 26 states, including information provided by Genesis HealthCare about its nursing homes in those states. The initial findings are supported by a similar study of nursing home data in 20 states led by researchers at Harvard Medical School.
They found homes where residents were infected with the coronavirus tended to be larger than other facilities, in urban areas and in counties with higher infection numbers. The data also showed the number of infections did not correlate to quality ratings or prior infection violations.
In Connecticut, eight nursing homes have had 30 or more coronavirus deaths. Of the eight, three have five-star ratings, two were given four stars, one had three stars, one had two stars and one had one star. All eight have been fined or cited by state or federal health officials in the past five years, according to an Associated Press review of regulatory actions.
The star ratings are based on the results of health inspections, staffing levels and the quality of resident care measures, according to the Centers for Medicare & Medicaid Services.
The virus has refocused attention to longstanding problems in the industry, including infection control lapses and staffing problems. In Connecticut as of May 14, there were 1,927 COVID-19-related nursing home deaths, about 60 percent of the more than 3,200 total deaths statewide on that date. Nearly 7,000 nursing home residents have tested positive for the virus.
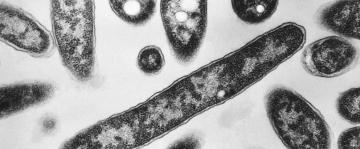
A key factor in the coronavirus entering nursing homes was not knowing, at the beginning of the pandemic, that asymptomatic people could spread the virus, said Mor and Dr. Sunil Parikh, an associate professor of medicine and epidemiology at the Yale School of Public Health. Testing and personal protective equipment also were initially in short supply.
The Connecticut nursing home with the highest COVID-19 death toll, at 54, is the Riverside Health & Rehabilitation Center in East Hartford, one of the largest nursing homes in the state with 345 beds. It has a four-star rating.
Riverside’s owner, National Health Care Associates, said the virus spread in the nursing home despite numerous precautions taken since the pandemic began including banning most visitors, screening staff for symptoms, limiting staff access to patient rooms and ending community meals among residents.
“We understood from the outset the grave threat that COVID-19 posed nursing home residents,” it said in a statement.
The operators of Abbott Terrace and Kimberly Hall North and staff say it may never be known exactly how the virus got into the homes, but once it was there, it spread quickly.
“It was like walking into a fire and no one knew how to put it out,” said Rosaina Rivera, a 41-year-old nurse at Abbott Terrace who tested positive for the virus in late March and recovered. “It was like an invisible demon possessing the building."
A fellow Abbott Terrace nurse and friend to Rivera, Ilkah Hernandez, died from the coronavirus last weekend, sending shock waves through the nursing home, she said.
The 205-bed Abbott Terrace isolated patients with symptoms early in the pandemic, Rivera said, but testing and N95 masks were scarce then. The nursing home also took staff members' temperatures and oxygen levels before they were allowed to work. No one knew then that people without symptoms could spread the virus, she said.
Staff members are frustrated by the low federal rating and negative publicity, Rivera said. Workers provide very good care, she said, but the home is large and its patients have more complex health and mental health problems — possible factors in having more reportable incidents than other nursing homes.
Timothy Brown, a spokesman for Abbott Terrace's owner, Athena Health Care Systems, said all violations found at Abbott Terrace were quickly corrected. He said staff are doing all they can to limit the reach of the coronavirus and are saving patients' lives every day.
An unannounced health inspection on April 29 at Abbott Terrace found infection control and social distancing violations — three residents in wheelchairs right next to each other not wearing masks, and one of them had tested positive for the coronavirus — according to a state Department of Public Health report released Monday. Nursing home officials told inspectors that staff were re-trained in mask and social distancing requirements.
The state has inspected all 215 nursing homes in the state during the coronavirus outbreak. Recent inspection reports for Kimberly Hall North and Riverside Health & Rehabilitation Center were not available Thursday.
Kimberly Hall North, the five-star nursing home, has 150 beds and is owned by Genesis HealthCare.
“When the virus does get into a nursing home, it does not discriminate,” said Dr. Richard Feifer, chief medical officer for Genesis HealthCare. “It impacts 5-star and 1-star buildings alike.”
The virus swept through the nursing home with alarming speed, said Cambar Edwards, a certified nursing assistant who has worked at Kimberly Hall North for 24 years. When the outbreak began, she said, N95 masks were in short supply and workers had to reuse them for days, even weeks.
“It’s like all hell breaks loose,” she said. “Because it is an invisible enemy, it was very hard.”