WASHINGTON -- Facing growing criticism, the Department of Veterans Affairs said Friday that it will not halt use of an unproven malaria drug on veterans with COVID-19 but that fewer of its patients are now taking it.
In responses provided to Congress and obtained by The Associated Press, the VA said never “encouraged or discouraged” its government-run hospitals in any way to use the drug hydroxychloroquine on patients even as President Donald Trump heavily touted it for months without scientific evidence.
Still, it acknowledged that VA Secretary Robert Wilkie had wrongly asserted publicly without evidence that the drug had shown benefit on younger veterans. The VA, the nation’s largest hospital system, also agreed more study was needed on the safety and effectiveness of the drug and suggested its use was now limited to extenuating circumstances, such as last-ditch efforts to save a coronavirus-stricken patient’s life.
In the first week of May, 17 patients had received the drug for COVID-19, according to VA data obtained by The Associated Press. The department declined to say how many patients had been treated with hydroxychloroquine for the coronavirus since the start of the virus outbreak in January, but a recent analysis of VA hospital data showed that hundreds of veterans had taken it by early April.
“VA has not endorsed nor discouraged the use of hydroxychloroquine in COVID-19 patients and has left those decisions to providers and their patients,” the VA said. “While all drugs have the potential for adverse events and some drugs in particular, like hydroxychloroquine, are known to have specific risks, when they are used carefully and judiciously, they can be managed safely.”
As of Friday, 11,883 veterans overall have been infected with the virus and 985 have died, according to VA statistics.
Responding to written questions from Sen. Jon Tester, the top Democrat on the Senate Veterans Affairs Committee, the department admitted it had no studies or evidence to back up Wilkie’s claim that hydroxychloroquine had shown effectiveness in younger veterans in particular.
“The use of hydroxychloroquine for COVID has dropped off dramatically,” the VA said.
Tester, who received VA’s responses this week, said he remained concerned about the safety of the drug after a recent analysis of VA hospital data showed the drug had no benefit.
“Any drug used to treat patients with COVID-19, especially veterans living with debilitating pre-existing conditions, must be proven safe and effective before it’s administered,” he said. “Given recent studies from both VA and other hospitals, hydroxychloroquine seems to fall short of those requirements.”
Major veterans’ organizations and congressional Democrats including Senate Minority leader Charles Schumer of New York had called on VA to explain why it allowed the use of an unproven drug on vets. Last week, a whistleblower complaint by former Health and Human Services official Rick Bright alleged that the Trump administration, eager for a quick fix to the onslaught of the coronavirus, wanted to “flood” hot spots in New York and New Jersey with the drug.
The analysis of hospital data, done by independent researchers at two universities with VA approval, was not a rigorous experiment. Researchers analyzed medical records of 368 older male veterans hospitalized with confirmed coronavirus infection at VA medical centers who died or were discharged by April 11.
About 28% of veterans who were given hydroxychloroquine plus usual care died, versus 11% of those getting routine care alone.
In its response to Congress, the department provided copies of some of its guidance issued to VA physicians on hydroxychloroquine from March to May. It made clear that hydroxychloroquine should be considered mostly for use in clinical trials or when medically appropriate after a full discussion with the patient about risks.
The VA did not explain the circumstances in which veterans in the recent analysis of hospital data were given the drug, only suggesting that “it is possible” they were prescribed as part of last-ditch efforts to save a patient’s life.
“Based on the principles of patient-centric care, it would be inappropriate to deny patients access to hydroxychloroquine under these dire circumstances,” VA wrote. It said it had followed the approach of the National Institute of Allergies and Infectious Diseases by “summarizing the medical literature regarding unapproved treatments for COVID-19 and making that available to VA clinicians in their shared decision-making with patients.” That guidance now includes preliminary studies on remdesivir, which has been federally approved for emergency use to treat COVID-19.
One VA document dated March 25 and obtained by the AP, notes to VA doctors that a few “very small cohort studies” showing possible “beneficial effects” but adds “these data have NOT been verified in randomized controlled trials and are extremely preliminary” and that prescriptions should only be made “after thorough consideration of all possible risks and benefits.”
Other VA memos, updated in April and early May, note the drug had not been federally approved for COVID-19 and had potential serious side effects.
The VA acknowledged to Congress it had placed bulk orders for hydroxychloroquine from Feb. 1 to April 23 for 6.3 million tablets worth $208,000 in anticipation of a possible shortage of the drug but that most of it was being used for approved uses, such as treating lupus and rheumatoid arthritis. It said it did not have breakdowns.
The department also said it planned further studies and clinical trials on hydroxychloroquine, including whether it could help prevent infection in veterans who were potentially exposed to COVID-19. It currently is in discussions with Novartis to have some VA facilities participate in a national clinical trial that will look at the effectiveness of hydroxychloroquine in combination with azithromycin in patients with moderate and severe disease.
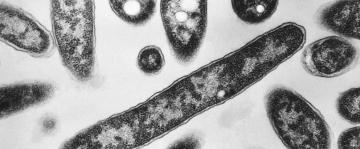
Hydroxychloroquine has long been used to treat malaria and other ailments. A few, very small preliminary studies suggested it might help prevent the coronavirus from entering cells and possibly help patients clear the virus sooner. But the FDA last month warned doctors against prescribing the drug for COVID-19 outside hospitals because of the risks of serious side effects and death.