If you’ve ever needed medication prepared in a special way, you may have needed to use the services of a compounding pharmacy. According to the U.S Pharmacopeia Convention, compounding is “the preparation, mixing, assembling, altering, packaging, and labeling of a drug” or device based on the prescription or orders of a provider.
Examples of compounding include preparing a special dosage of a medication; preparing a flavored version of a medication, whether it’s mixing it into a syrup for a child or a chewable treat for a pet; reformulating the medication to get rid of any non-essential allergens, such as lactose; or changing the form of a medication, such as mixing it into a liquid form for patients who can’t swallow pills.
Compounding pharmacies exist because sometimes the commercially available medications just won’t work for a patient’s needs. That’s when a compounding pharmacy (and pharmacist) can step in. Although most pharmacies (and pharmacists) can do a limited amount of compounding, the more specialized orders often go to places that specialize in compounding, where the pharmacists have specialized tools, training, and ingredients available.
How to use a compounding pharmacy
A compounded medicine is prepared specially for an individual patient, and requires a prescription. Of the approximately 56,000 pharmacies in the U.S., about 7,500 of them are dedicated compounding pharmacies. To find a compounding pharmacy near you, you can search the Alliance For Pharmacy Compounding’s website locator. If your doctor wants to prescribe a medication that needs to be filled by a compounding pharmacy, they likely will also have a local recommendation.
As the Alliance For Pharmacy Compounding suggests, when choosing a compounding pharmacy, it’s advisable to ask about quality standards, including whether they adhere to the United States Pharmacopoeia standards; the training of the pharmacy staff; the compounding process by which your medication will be prepared, including sterile procedures for any eye drops or injections; and whether they are accredited by the Pharmacy Compounding Accreditation Board.
What to be aware of
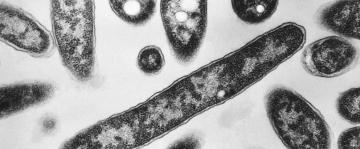
There have been a number of past warnings and controversies due to unsafe medications being prepared by compounding pharmacies, including a 2012 fungal meningitis outbreak, where 753 patients in 20 states developed a fungal infection after being injected with a contaminated medication that had been prepared by a compounding pharmacy. Since then, the FDA has periodically issued alerts about contaminated products that have been prepared in compounding pharmacies.
Most recently, the FDA issued a warning about customized preparations of semaglutide, which is the active ingredient found in Ozempic and Wegovy, that are being sold by compounding pharmacies at lower costs, due to an FDA loophole saying that patented drugs can be compounded during shortages.
However, as the FDA recently warned, there are a number of risks associated with using these compounded preparations, as there have been adverse events reported in patients using them. The company that manufactures semaglutide does not sell it in a form that can be used by compounding pharmacies; instead, these pharmacies may be using research-grade semaglutide salts. The FDA says they “are not aware” of any way this can be done legally—meaning compounded “Ozempic” is likely not the real deal.
As the FDA notes, one of the major differences between a commercially available medication and a compounded medication is that the quality standards are different. A commercially available medication is required to go through the FDA approval process, and is subject to a number of quality control regulations, whereas a compounded medication is not considered FDA-approved. A compounded medication can be made of an FDA-approved medication, but the compounding process has a different set of rules and regulations, which are not subject to the FDA approval process.