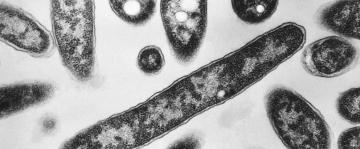
When I wrote about what it means to be immunocompromised in early March of this year, I was itching to get vaccinated. People are immunocompromised for a variety of reasons—genetics, age, metabolic diseases like diabetes, and immune-suppressing medications taken for conditions including autoimmune diseases, organ transplants, and cancer—but what we all have in common is a weaker immune system, making us more vulnerable to infections like COVID-19. The vaccine could be a lifesaver for us.
I was elated when I received my second Pfizer dose on April 12, hopeful I could end my year-plus of near-total isolation. Before the week was over, however, multiple reports appeared showing that immunocompromised people were not producing antibodies after getting vaccinated. Hope suddenly turned into fear.
Less than a month later, on May 13, the CDC released new mask and distancing guidelines. Fully vaccinated people with healthy immune systems (aka the immunocompetent) can now safely resume pre-pandemic behavior indoors and out. In contrast, the CDC’s advice for the immunocompromised is that we might need to continue masking and social distancing even if vaccinated, because we might not have sufficient immunity to protect us from a severe case of COVID-19. These contradictory guidelines have implications for everyone, not just immunocompromised people.
If you have a healthy immune system and adopt the new CDC guidelines, for instance, you could potentially expose immunosuppressed family, friends, colleagues, and clients to COVID-19 even if everyone is vaccinated. Moreover, the best estimate we have for the number of immunosuppressed Americans—approximately 8.5 million—is an undercount. So, you might be putting someone in your circle at risk who doesn’t realize they are immunocompromised. That someone might even be you.
The good news is that the science is increasingly clear on which particular immunosuppressive conditions and medications are most likely to lower vaccine immunity, even if the crucial question—how much immunity is enough to protect someone from severe COVID-19—remains unknown.
Here’s what the science currently says about vaccine immunity and immunocompromised people, and how you can use that knowledge to protect yourself and immunocompromised friends and family in light of the new CDC guidelines.
There’s no test that can tell you for sure if your vaccine worked
Vaccines work by stimulating the immune system to respond to a weakened or benign version of a virus. This response produces antibodies and rallies virus-killing cells to eliminate an infection before it has time to wreak irreparable damage. Both common sense and science tell us that the more robust your immune system, the more effective a vaccine will be at giving you immunity. Vaccine immunity is usually measured by testing the blood for the presence of antibodies, and a recent study concludes that antibody levels are a good indicator of COVID-19 vaccine immunity specifically.
That said, scientists have consistently urged people not to get COVID-19 antibody tests to check their vaccine immunity, for three main reasons. First, the most common antibody test doesn’t look for the specific antibody stimulated by the vaccines but, rather, for a protein produced only by an actual COVID-19 infection.
Upon closer inspection, the studies on vaccine immunity in the immunocompromised are not all doom-and-gloom.Second, antibodies are not the only marker of COVID-19 immunity. Healthy people have recovered from COVID-19 infections without producing antibodies, because immune cells known as T cells picked up the slack. One reviewstudy, in fact, suggests that a robust T cell response not only compensates for a lack of antibodies, but also might be the most important factor in fighting off COVID-19 infection. Unfortunately, many of us who are immunocompromised have fewer or less functional T cells, so this news is not completely reassuring.
Finally, the million dollar question of “how much immunity is enough”—that is, how many antibodies or COVID-19 destroying T cells you need in your system to be protected—depends on so many variables in our incredibly individualized and complex immune systems that a valid answer remains elusive.
However, upon closer inspection, the studies on vaccine immunity in the immunocompromised are not all doom-and-gloom.
What we know about certain medical conditions
“I’m of the strong opinion that many people have been worried unnecessarily [by the media reports],” Dr. Meena Bewtra, an assistant professor of gastroenterology and epidemiology and IBD specialist at the University of Pennsylvania, told me. As more studies come out, we’re learning that fears most immunocompromised people in general would struggle to make antibodies are not coming to fruition. Here’s a little of what we know so far:
Inflammatory bowel disease
Dr. Bewtra herself is one of the principal investigators of a study that has found vaccine antibodies in 96 percent of nearly 500 Americans with inflammatory bowel disease (IBD), most of whom are on some form of immunosuppressants. “What we’ve seen here [for IBD patients] is very reassuring,” she said.
Transplant recipients
Thus far, the research has identified a few immunocompromised groups who are less likely to produce antibodies post-vaccination. One is transplant patients, especially those who take a drug called mycophenolate (brand name: Cellcept). One study found only seven percent of kidney recipients having the specific spike protein antibody created by the Pfizer and Moderna mRNA vaccines are designed to produce, whereas another study recorded a more encouraging—but hardly celebratory—54 percent. Heart and lung transplant recipients showed similarly low percentages: Only 14 percent of heart recipients and 18 to 25 percent of lung recipients had antibodies. People with blood cancers (leukemia and lymphoma) also appear to have less immunity, though the percentage of people with antibodies varies significantly—from 39.5 to 83 percent—depending on cancer type, treatment status, age, and other factors.
Rheumatic disorders
Two U.K. studies found fewer vaccine antibodies in people with rheumatic and musculoskeletal disorders taking rituximab (brand name: Rituxan) and IBD patients taking infliximab (brand name: Remicade). However, these U.K.-based studies measured antibodies after only one of two vaccine doses, because its vaccination program chose to delay second doses in order to vaccinate more of the population. Encouragingly, the people in the Remicade study who got their second dose had antibody levels similar to that of the general population.
Everybody else
Still, these studies cover only a fraction of immunosuppressive conditions and treatments, and therefore provide definitive data for only a fraction of immunocompromised people. Both Pfizer and the National Institutes of Health (NIH) are conducting broader studies on vaccine immunity and the immunocompromised, but findings likely won’t be available until next year. That’s why the CDC guidelines—that you may need to continue masking, because you might not have immunity—are so frustratingly, unhelpfully broad.
As Professor Candida Moss, who recently wrote about the difficulties of navigating the new guidelines as a kidney transplant recipient, told me, “There’s just not enough information, even among the transplant community, much less when you read a CDC infographic which clearly doesn’t apply to you.”
What immunocompromised people can do to protect themselves
The most important thing we immunocompromised people can do to protect ourselves from COVID-19 is to be healthy, and that means staying on our immunosuppressants. (You thought I was going to say get vaccinated, right?)
Getting vaccinated is the second most important thing we can do.Don’t get me wrong: Getting vaccinated is the second most important thing we can do. However, both Dr. Bewtra and Professor Moss mentioned anecdotal evidence of people considering stopping their medications to boost their immune system before getting the COVID-19 vaccine—something I briefly considered.
In short, the answer is no; not only does active disease tax our already weakened immune system, but also we can end up exposed to COVID-19 if hospitalized or on far more aggressive immunosuppressants than the ones we’re currently taking. (However, the American College of Rheumatology does have recommendations about skipping or delaying dosages of specific medications if you are relatively healthy.)
No matter what your health and vaccination statuses are, you should reach out to your doctor, in particular any specialist who treats your particular condition or has prescribed you immunosuppressants. (If you’re not sure if the medication you’re on is immunosuppressive, check out this list.)
Admittedly, this advice is often easier said than done. The earliest appointment I could get with my specialist was a month away. Moreover, many immunocompromised people lack access to specialists or even primary care physicians because of systemic problems that disproportionately affect people with disabilities, minorities, the poor, and rural Americans.
If you have an internet connection, however, many non-profit organizations have regularly updated information and guidelines on vaccine immunity for specific conditions. On sites like the Leukemia and Lymphoma Society, the Crohn’s and Colitis Foundation of America, Creaky Joints (for patients with arthritis), or the American Society of Transplantation, you can find links to the latest studies, detailed FAQs, and even opportunities to join ongoing studies that can set you up with that elusive vaccine-specific antibody test for free.
“While I don’t think everyone has an obligation to create accessible spaces for the immunocompromised in every occasion,” Moss said, “I think they do have an obligation to communicate.”What everyone else can do to protect the immunocompromised
The best thing healthy people can do to support the immunocompromised population is to get vaccinated. Period.
However, continuing to wear a mask and practice social distancing in most indoor spaces is almost as important, whether or not you’re vaccinated.
“It’s not that I think everyone should keep masking everywhere, forever,” said Moss, who works from home in New York City, “[but] it would be nice if essential services like grocery stores, public transportation, doctor’s offices, pharmacies—places that you have to go to—could have masking.”
Masking in public spaces like hotel and apartment lobbies also protects staff who can’t leave their posts. “You don’t know what kind of health conditions the people working in those spaces have,” Moss said. While the science suggests that fully vaccinated people spread less virus if exposed to COVID-19 than non-vaccinated people, erring on the side of caution is the surest way to prevent immunocompromised people in your life from suffering hospitalization, long-term effects, or even death.
Finally, a little more intention when planning informal and formal gatherings can make a huge difference. Be specific about whether an event will require masks, distancing, or vaccination so that people can make the right decisions for their personal safety. Whenever possible, go outdoors or hybrid. “While I don’t think everyone has an obligation to create accessible spaces for the immunocompromised in every occasion,” Moss said, “I think they do have an obligation to communicate.”
The biggest challenge is getting the information to the people who need it
In the course of writing this article, I went from the despair of believing I likely had little to no vaccine immunity to a stunned relief that the odds are actually in my favor. While speaking to Dr. Bewtra gave me hope for my personal health, my conversation with Professor Moss reminded me that my behavior has an impact beyond my immediate circle. When I do re-enter society, I want to do so compassionately, in the knowledge that not everyone can move safely in this brave new world.
I will therefore mask indoors in essential places, around essential workers, and around children. (I’ll probably mask outdoors, too, but that’s my anxiety talking and not the science.) I won’t make assumptions about why those around me are or aren’t wearing masks, though I’ll remove myself from a space if necessary to feel protected.
Most of all, I’ll be more open about this invisible disability of immunosuppression. If the pandemic has taught us anything, it’s how interconnected we all are. What hasn’t spread as successfully is information to the people who need it. This article can’t fill those gaps, even if it goes viral (pun intended). Just like the COVID-19 vaccine itself, however, the information in it could be a lifesaver.